
Medicaid Transformation Podcast: Interview with Dr. Marc Harrison, President & CEO at Intermountain Health
AVIA
Insights
Sarah Carroll, Director, Medicaid Transformation Project, AVIA

On January 9, the world learned that “hotspotting,” the Camden Coalition’s highly respected complex care model, did not perform better than standard care in a randomized controlled trial. Social media sites reverberated with a mix of surprise and speculation.
Hotspotting had produced tremendous community collaboration, compelling anecdotes of individual success, and improvements in primary care utilization. In spite of all that, people in the intervention group had about the same rates of 180-day hospital readmissions as those without intensive care support.
Study authors, Coalition leaders, and healthcare reporters had plenty to say about the trial’s limitations and community challenges, but there is enormous opportunity to take this great model and make it better, with digital. This is the work the AVIA Innovator Network is doing with the Medicaid Transformation Project (MTP), a national effort with 30 health systems to transform healthcare and address related social needs by implementing digital solutions and innovative care models.
Their typical client has experienced multiple emergency department (ED) visits and hospital admissions in a single year, has at least two chronic conditions, uses several medications, has difficulty accessing services, and lacks social support. Many also have a mental health condition, substance use disorder, and are homeless. Nurses, social workers, and community health workers meet these clients shortly after discharge, schedule primary care visits, and continuously support them at home to meet a variety of needs. The coalition also reduces fragmentation by collaborating with non-traditional partners, including the justice and education systems, policymakers, and payers.
Unfortunately, the study’s average intervention time was 92 days with a key performance indicator of a readmission within 180 days. We are left to wonder if the two groups demonstrated any other meaningfully different experiences or outcomes in those 92 days, and question if 92 days is enough time to support the most challenging and complex conditions developed over a lifetime. Nonetheless, the Camden Coalition represented an important step forward in complex care management and coordination.
Camden Coalition leaders and investigators identified a number of barriers to success, including a lack of housing, communication tools, and behavioral health providers. They also questioned if the study design precluded success among certain sub-populations. The Medicaid Transformation Project has vetted a number of digital solutions that could have helped the team overcome these obstacles, such as:
Moreover, digital solutions could enable a number of other hotspotting goals for a longer period of time, such as more efficient provider communication, greater staff productivity, deeper patient engagement, and lower cost of care. Examples include:
MTP members have demonstrated a number of compelling operational, financial, and population health gains by selecting one solution, or layering solutions in a product development approach for complex populations. One example is the digitally enabled Geisinger at Home model. This model currently combines a multidisciplinary team with post-discharge telehealth visits, Bluetooth scales for weight monitoring, and digitally transmitted wound images. To date, the model has improved patient quality of life, reduced ED visits by 35% and hospital admissions by 40%, and saved, on average, nearly $8,000 per patient served. (1)
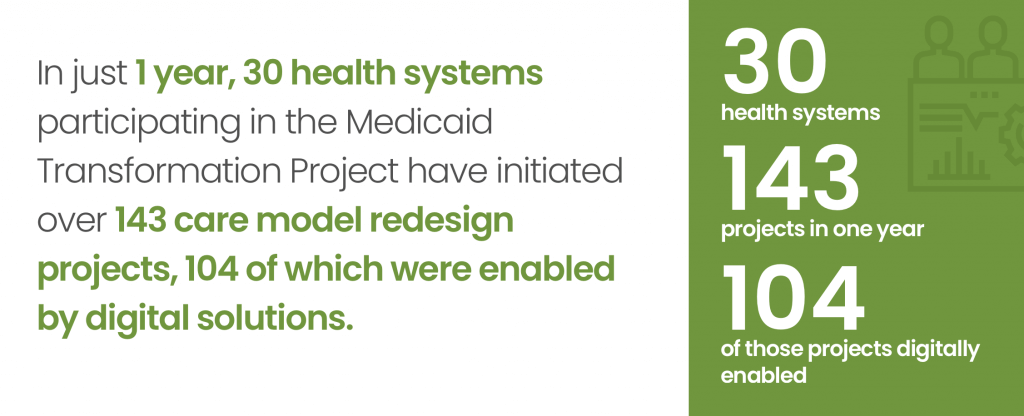
Investors have poured nearly $40B into digital health start-ups since 2011. The AVIA Network was built to de-risk and accelerate decision making. Since launching MTP in 2018, we have reviewed over 444 digital solutions to identify 42 best-in-class partners with demonstrated impact supporting complex patients. AVIA supports the Network with resources to compare solutions, build the business case, showcase success stories, and share recommendations to scale. The progress is inspiring. In just one year, 30 participating health systems have initiated 143 care model redesign projects – with 104 being digitally enabled – to increase access, reduce avoidable utilization, and improve health outcomes for individuals with complex needs.
The AVIA Network is committed to testing new ideas, sharing what works, and incorporating lessons to achieve impact at scale. Are you interested in learning more and getting involved? Join us in Chicago this March for our Community-Centered Care Action Forum, a convening of health systems, health plans, solution companies, policymakers, and thought leaders to build on what we’ve learned to advance complex care models and population health. Learn more at www.aviahealthinnovation.com or email us at contact@aviahealthinnovation.com.