
“New work”: Defining your healthcare automation & operations strategy
AVIA
Insights
Marc Griffin, Vice President, and James Cao, Senior Manager, Center for Operational Transformation, AVIA
To survive the rapidly shifting economic climate during the pandemic, health systems have made drastic operational shifts to safely serve patients while accounting for revenue loss. The importance of becoming a truly digital operation has never been clearer: A Blackbook survey found 80% of CFOs think automation is an absolute and immediate need for long-term survival.
In Q1 of 2020, telehealth companies saw a VC funding boom of $788 million, but attention needs to be paid to solutions beyond virtual visits and patient portals. Analysis has found 36% of healthcare tasks could be automated, and 25% of provider and staff labor is currently focused on administrative tasks. In a 2019 AMA survey, 86% of physicians described the administrative burden associated with prior authorizations as high or extremely high.
Digital, in short, could transform your organization’s operations. One immediate and high-impact opportunity is leaning into areas of your organization’s revenue cycle where digital technology is mature with proven results on improving the bottom line and patient and provider experiences.
The 2019 CAQH Index Report found that of the $40.6 billion spent on administrative transactions in the revenue cycle, $13.3 billion or 33% of existing annual spending could be saved by completing the transition to fully automatic electronic processing.
Additionally, an internal AVIA analysis found a sample health system with net patient revenue of $2 billion could see a $25.2 million* financial impact from digital healthcare reimbursement solutions, including increasing patient self-pay collections and reducing denials and write-offs.
When creating a digital healthcare reimbursement strategy, first consider your organization’s strategic priorities. While digital can improve all parts of your revenue cycle, it’s important to focus on the areas of your organization where improvement would best align with your business needs, KPIs, and goals.
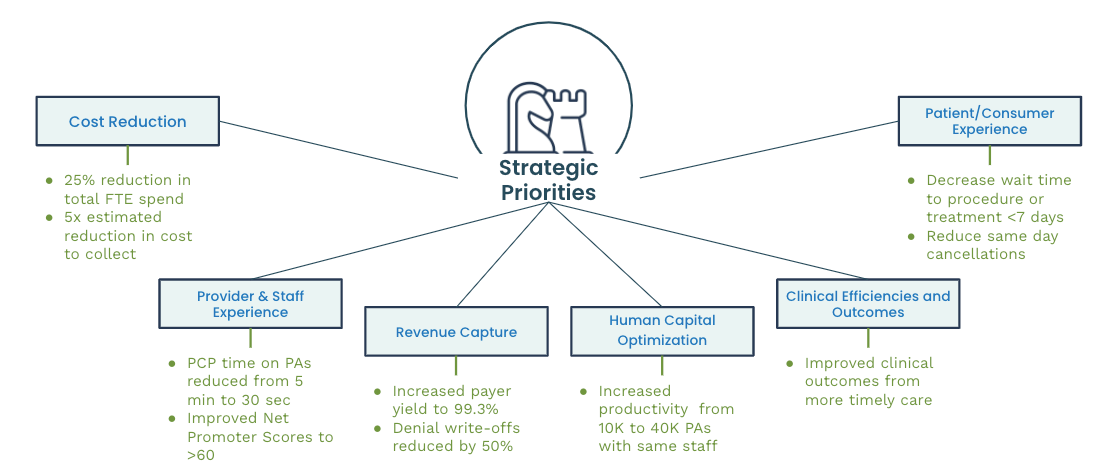
Priority areas to consider include:
Under the umbrella of revenue cycle management, there exists a broad spectrum of functions, from cost estimation to prior authorization. With so many moving parts, it’s easy to get misdirected or focus digital efforts on an area that may not drive the MOST significant impact for your organization.
Experts at AVIA’s Center for Operational Transformation identified four areas within your revenue cycle where digital can make an outsized, lasting impact on both patient experience and financial outlook:
When making the business case for digital healthcare reimbursement solutions, know the benefits extend beyond improving your organization’s bottom line. Digital revenue cycle solutions in the four categories listed above can also make a powerful impact on patient experience and care.
For example, financial clearance tools can provide personalized estimates and financial assistance to patients examining the cost and coverage of a certain procedure. Prior authorization solutions can help patients and hospitals avoid same-day cancellations and prevent unexpected bills for patients. Together, these solutions can transform the patient experience at your organization. They can also ensure patients receive quality and timely care while reducing or preventing the stressful experiences of waiting on call centers and navigating unexpected bills.
Digital solutions can transform your organization’s healthcare reimbursement strategy, driving revenue and increasing patient experience. Starting to incorporate digital into your organization’s operational capabilities can be daunting, from aligning stakeholders to developing an action plan.
Experts at AVIA’s Center for Operational Transformation are here to help. We partner with leaders at organizations like yours in our Member Network to apply our insights, proven tools, and vetted solution companies to tackle your organization’s unique digital reimbursement challenges. To learn more about what a partnership with AVIA looks like, contact us today and join the digital reimbursement conversation on our free platform, AVIA Connect.
*All cause denial write-offs 2.1% of NPR, financial clearance denials write-offs 0.76% of NPR, prior authorization denials write-offs 0.46% of NPR, and denials management write-offs 0.5% of NPR