Hospitals and health systems looking to foster big data and health IT innovation are running up against some familiar organizational challenges.
September 22, 2017 – Productive partnerships and more effective management processes are a fundamental requirement for hospitals and health systems seeking to harness their big data assets for digital innovation, says a new survey conducted by the American Hospital Association (AHA) and AVIA.
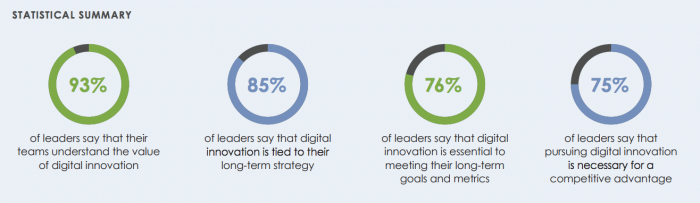
While than 75 percent of executives participating in the poll believe that digital innovation is the lynchpin in their long-term strategies for financial and clinical success, 54 percent admit that the time they spend on digital innovation projects is not being used efficiently.
The chronic diseases of project success, including lack of funding, a scarcity of talent, and underdeveloped governance skills, are afflicting the majority of hospitals and health systems, leaving many organizations unclear about the path ahead.
“The term innovation is used frequently and inconsistently,” the report notes. “At its most basic level, innovation means introducing a new idea, device, or method. To be innovative is putting something new into practice, typically with the intent to improve upon previous methods. Particularly within healthcare, innovation is a fluid and evolving field.”
The current definition of innovation is centered on digital solutions, including EHRs, predictive analytics, business intelligence tools, and other systems driven by big data.
READ MORE: Leveraging Business Intelligence for Healthcare Management
Ninety-three percent of the 300 respondents to the survey believe that their teams understand the value of digital innovation, when performed correctly, while 85 percent say that the development of their health IT infrastructure is a core component of their organizations’ long-term strategies.
Source: AHA / AVIA
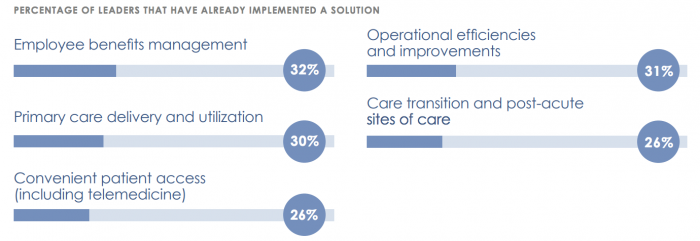
Top clinical priorities include primary care delivery innovation, health information exchange, patient engagement and access tools such as telemedicine, and solutions to incorporate patient-generated health data in the decision-making process.
On the financial and administrative side, executives are eyeing big data analytics and business intelligence tools to address network leakage and referral management, employee benefit management, and other operational efficiencies.
“It’s clear that hospitals recognize and embrace the importance of digital innovation,” said Maryjane Wurth, AHA executive vice president and chief operating officer. “Our hope is that by collecting and sharing this data about their aspirations, priorities and challenges we can accelerate the pace of change in the field.”
Source: AHA / AVIA
Quality improvement is the ultimate goal for these executives, who cited quality and safety as their top two metrics for success.
READ MORE: Turning Healthcare Big Data into Actionable Clinical Intelligence
Cost reductions came in third, followed by improvements to patient satisfaction. A better provider experience was last on the list, but still a critical measure of the effectiveness of their digital investments.
Fulfilling these ambitions will mean overcoming several of the longest standing industry challenges.
Seventy percent of executives believe that their IT departments do not have the resources to support an effective digital transformation plan, and 52 percent are holding off on projects due to a lack of available capital.
Regulatory uncertainty is giving pause to 37 percent, while 60 percent are hesitating due to insufficient ROI from previous attempts at implementing new tools and processes. Only a quarter said they had derived full value from their solutions in the past.
Many of these failures may be attributed to insufficient organizational governance principles, acknowledged the participants.
READ MORE: The Difference Between Big Data and Smart Data in Healthcare
“It’s extremely difficult to realize a meaningful ROI when implementation processes are incomplete or inconsistent,” the survey says. “A lack of dedicated resources, authority, and budget can impede true collaboration and restrict innovation acceleration.”
Just 45 percent have standardized processes in place to assess whether or not to pilot a new digital solution. Half of the time, an identified need does not receive a pilot. Only 51 percent of organizations have established metrics for deciding if a pilot is successful enough to be brought to scale.
And despite the fact that nearly 70 percent of leaders believe that constant experimentation is critical for moving forward, many believe that the ability to do so is simply not in their DNA.
“Innovation isn’t a core competency of many healthcare organizations,” observed one participant. “The industry needs help identifying options for advancing meaningful innovation and building the structure needed to support it.”
Forging partnerships within the community, such as investing in health information exchange (HIE) network and improving transitions of care with business partners, is a high priority for most health systems.
“[We need] more thought leadership about innovation; convening groups to discuss, identifying metrics to track success, forward looking views on innovation, [and] practical implementation of solutions,” said a participant.
Collaborating closely on the technology front is also important for achieving better outcomes. But many health systems are angling to be the leaders rather than the ones seeking out the expertise of others.
Twenty-nine percent of organizations – including half of academic medical centers and 72 percent of hospitals with more than 400 beds – are planning to invest or have already created “innovation centers” that include dedicated personnel and resources for technical and strategic development.
“Built correctly, a standalone innovation center can be nimble, resilient, powerful, and a key to driving scaled, impactful digital innovations,” the report asserts.
A successful innovation center can produce immediate and impactful results. Organizations that have gotten their digital development programs right can achieve meaningful ROI up to 52 percent faster than health systems struggling to realize their big data visions, the survey found.
A dedicated funding pool for health IT development or a mechanism for funding innovation outside of the traditional budget cycle can each accelerate the process by 17 percent. Carving out a portion of each service line’s budget to address specific issues can help providers move 22 percent faster.
Securing sufficient technical skills and IT resources can provide a 23 percent boost in time and efficiency.

Source: AHA / AVIA
All together, these strategies can shorten a 23-month development cycle in a 12-month project, allowing organizations to attack a broader range of issues much more quickly than their peers.
“Top performers are nimble and confident, removing operational barriers by dedicating funding and resources to innovation,” the AHA said. “Just as significant, they institute specific processes like flexible budget reviews and workflows with clear decision rights to allow innovation to thrive. These process improvements strongly correlate with the agility and speed of innovation.”
“Knowledge sharing, collaboration, and best practices can help galvanize action, crystallize innovation priorities, and accelerate transformation across the field.”
